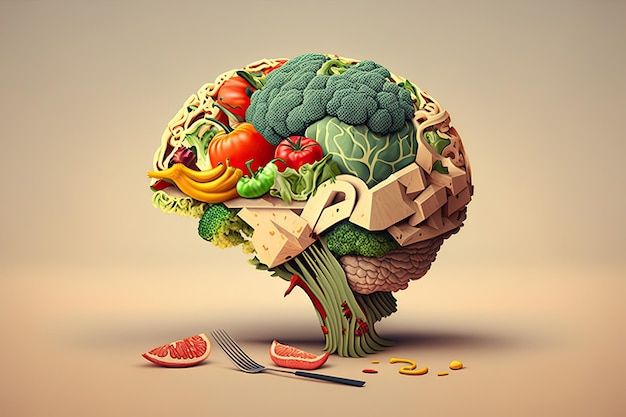
Psychiatric Nutrition, explained:
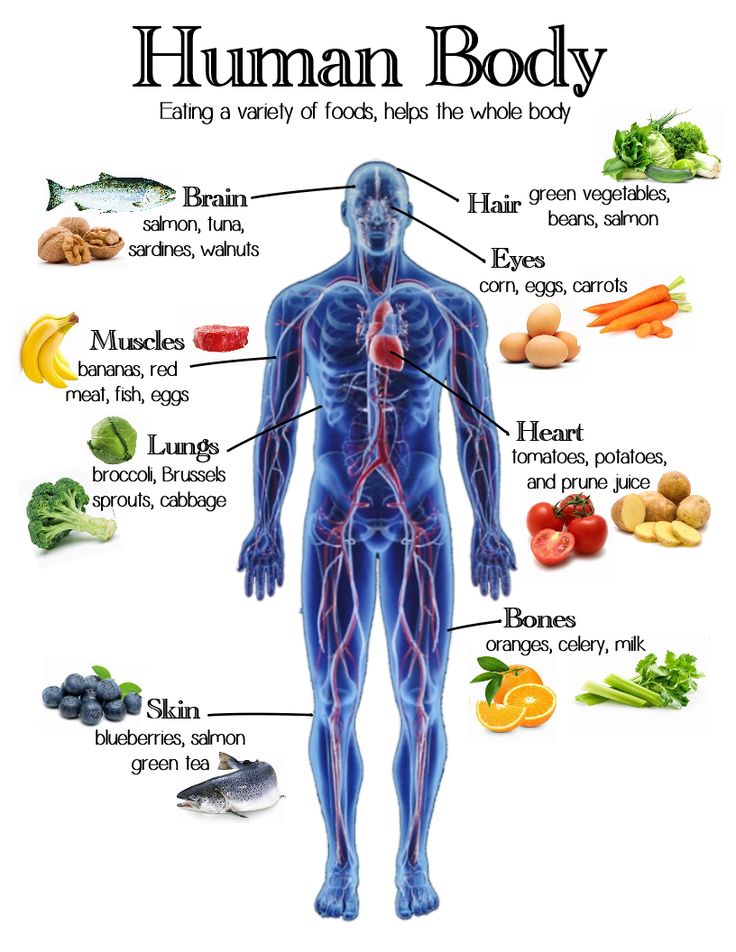
As has been well known throughout the millennia of humanity, from the oldest sciences such as Ayurveda, Chinese medicine, the Hippocratic school of medicine in ancient Greece, and other ancient disciplines, nutrition is essential for our health and well-being because it is what gives us the energy day by day to live and give our body what it needs to function, so food and everything that enters our mouths reaches every corner of our cells, it is something that has a very strong impact. deep in us. Therein lies the importance of having a good diet and it is now scientifically proven how it can affect our minds.
What is Psychiatric Nutrition?
Psychiatric Nutrition is a new scientific field, and it is born from two large branches of health sciences, nutrition and psychiatry. What this new branch of science can offer is quite promising in terms of offering better treatment and new opportunities to people living with mental illness, something quite common today everywhere.
But where exactly does this branch come from and what is it scientifically based on? A consistent evidence base of observational literature has been created that affirms and confirms that the quality of people’s diets is related to their risk of common mental disorders , such as depression . And not only is that confirmed, but it happens the same in all countries and age groups. This means that dietary changes are being implemented for the prevention and treatment of depression.
At the same time, the information suggests that nutraceuticals may be useful as a complementary treatment for mental disorders and as monotherapies for conditions such as ADHD , which is also known as attention deficit.
There are new discoveries and research focused on understanding the biological pathways that regulate the observed relationships between diet, nutrition and mental health and how they target the immune system, oxidative biology, brain plasticity and the microbiome-gut-brain axis. of high importance for nutritional interventions.
But something to keep in mind is that this field is still quite limited by lack of research, lack of data, and methodological problems, such as heterogeneity, residual confounding, measurement error, and other challenges in measuring and ensuring dietary adherence in studies. of intervention. Another thing is that nutraceutical and “psychobiotic” interventions must be carried out in a scientific and rigorous manner that also examines the predictive factors of the response that the treatment will have.
When was Nutritional Psychiatry born?
It is something quite recent, it began with simple studies such as the usefulness of omega 3 and folic acid supplementation in mood disorders that were carried out in past decades. It also arises from pioneering studies that concluded to connect diet quality with common mental disorders such as depression and anxiety. In the latest research, there has already been a focus on isolated nutrients.
The term “ nutritional psychiatry or psychiatric nutrition ” was used precisely to promote a new field of research focused on the development of more scientific content to enrich this potential field. It has been a somewhat difficult path since it emerged since a determining and definitive study model has not been established. What is a fact is that the relationship between healthy and unhealthy diets and mental health is compelling.
Low intake of healthy, nutritious, high-fiber foods and high intake of processed, sugary, and fat-laden foods are associated with poor mental health.
Existing evidence largely supports a causal relationship between diet quality and depression based on the Bradford Hill criteria: the consistency of concordant findings and effect sizes across cultures, genders, and age groups with multiple methods used to evaluate the quality of diet and mental health.
What recommendations exist today for Psychiatric Nutrition?
The intervention that includes the ‘ModiMedDiet’, concluded that in a very general way a diet that is rich in vegetables, fruits and whole grains, with an emphasis on increasing the consumption of fatty fish, extra virgin olive oil, legumes and raw unsalted nuts is good for our mental health.
Bipolar disorders:
They reviewed the scientific literature on nutritional supplements for major depressive disorder and disorders including bipolar depression and found little support for these as monotherapies, but concluded that there was evidence of the usefulness of folic acid, S-adenosyl-methionine (SAM), omega-3 fatty acids and L-tryptophan as complementary therapies.
Depression
A more recent systematic review and meta-analysis of nutraceuticals as complementary therapies for depression confirmed the efficacy of SAMe, omega-3, methylfolate, and vitamin D, but provided only limited support for zinc, folic acid, vitamin C, and tryptophan. . Another study also conducted a recent systematic review and meta-analysis of the literature on the short- and long-term impact of vitamin B12 and folate as a treatment for depression. It was concluded that the evidence did not support these B vitamins as a short-term treatment, but that they may offer some long-term preventive potential.
Schizophrenia and bipolar depression
What has been found regarding nutritional supportive treatment for schizophrenia and bipolar depression is by other nutraceuticals with methods of action focused on addressing the pathophysiological aberrations that characterize many psychiatric disorders, such as inflammation, oxidative stress, reduced neurogenesis and mitochondrial dysfunction, have shown great promise. For example, N-acetyl cysteine (NAC), a bioavailable amino acid that upregulates glutathione and modulates glutamatergic, neurotropic, and inflammatory pathways, has shown preliminary efficacy as an adjunctive treatment in schizophrenia and bipolar depression, but not in major depressive disorder.
What are the Metabolic Pathways Evidenced by which Psychiatric Nutrition works?
Now we will talk about which are the metabolic pathways involved in mental illnesses and that can be altered with diet. This is an overview of the evidence for the main pathways that have been studied to date in psychiatric nutrition . Although described as distinct pathways, it is likely that these pathways overlap synergistically and interact with each other.
Inflammation
Low-grade chronic, characterized by an increase in proinflammatory cytokines and acute phase proteins, is implicated in the development of depression, schizophrenia, and bipolar disorder. The causes of this inflammation are multifaceted and include several lifestyle factors, such as psychological stress, smoking, obesity, lack of sleep and, of particular relevance to the present discussion, poor diet. Results from large observational studies suggest that healthy dietary patterns , such as the Mediterranean diet, that are higher in polyunsaturated fatty acids (omega 3 and omega 6), fiber, fruits and vegetables are associated with lower levels of inflammatory markers . Furthermore, Mediterranean dietary patterns significantly improve markers of inflammation in intervention studies.
Oxidative stress
Oxidative and nitrosative stress are implicated in several chronic diseases and appear to be relevant to mental illnesses. Schizophrenic populations have low levels of glutathione in the brain, glutamate metabolism is also disorganized and oxidative stress is increased. Similar results are reported in depressed populations, with higher levels of oxidative stress markers observed, as well as lower levels of antioxidants, such as vitamin E, vitamin C, coenzyme Q10 and glutathione, compared to healthy controls. Furthermore, a recent meta-analysis of 115 studies reported lower antioxidant capacity in depressed patients during acute episodes. Given the abundance of antioxidant compounds present in foods such as fruits and vegetables, this is a pathway that could be modulated through dietary means.
Brain plasticity
Neurogenesis , particularly in the hippocampus, is associated with learning, memory , and mood regulation, while altered neurogenesis is implicated in mental illness. Brain-derived neurotrophic factor (BDNF) as well as other neurotrophins (e.g., bcl-2 and vascular endothelial growth factor) are suggested to mediate hippocampal neurogenesis.
There is currently limited clinical investigation of the effect of diet on this pathway; However, preliminary evidence supports the role of diet in improving BDNF levels. For example, a 4-week dietary intervention to increase consumption of carotenoid-rich fruits and vegetables (eight servings daily) in people with schizophrenia resulted in higher serum levels of BDNF than in the control group. Furthermore, epidemiological research in older adults has shown an association between poor diet and reduced hippocampal volume . In addition to possessing antioxidant and anti-inflammatory properties, nutrients, such as omega-3 fatty acids, polyphenols, L-theanine and vitamin E, can also stimulate neurogenesis , while energy-dense diets high in fat and sugar They simply prevent this process. Junk food is an example of foods that are quite bad for this type of condition.
Mitochondria Dysfunction
Decreased mitochondrial energy production, size, and distribution are associated with depression, schizophrenia, and may be particularly relevant to bipolar disorder. These changes could be the result of reduced antioxidant capacity and a proinflammatory cytokine-mediated increase in mitochondrial-derived oxygen and nitrogen free radicals, suggesting mitochondrial dysfunction driven by inflammation and oxidative stress. Dietary and nutraceutical compounds such as coenzyme Q10, α-lipoic acid, carnitine, creatine, resveratrol, NAC and some other antidepressants regulate mitochondrial respiratory function in animal models.
Microbiota, Fermented foods and Mental Health
The Role of the intestinal microbiota is something that has been known for a short time, this was a decade ago, before scientific hypotheses, there was talk of the intentional manipulation of the intestinal microbiota and that this could provide therapeutic value to humans with depression and with fatigue states. However, many of the proposed mechanisms have already confirmed that fermented foods have microbes that are beneficial and could influence mood or fatigue.

Here is a short list of why fermented foods help:
- Direct protection of the intestinal barrier.
- Influence on local and systemic antioxidant status, reduction of lipid peroxidation.
- Direct neurochemical production, produced by microbes, for example, gamma-aminobutyric acid ( GABA ).
- Indirect influence on neurotransmitter or neuropeptide production.
- Prevention of stress-induced alterations in general in the intestinal microbiota.
- Direct activation of neural pathways between the intestine and brain.
- Limitation of the production of inflammatory cytokines.
- Modulation of neurotrophic chemicals, including brain-derived neurotrophic factor.
- Limitation of carbohydrate malabsorption.
- Improved nutritional status, for example omega-3 fatty acids, minerals, dietary and phytochemicals.
- Limiting bacterial overgrowth of the small intestine, promotes a healthy balance.
- Reduction of the load of amines or uremic toxins;
- Limitation of gastric or intestinal pathogens (e.g. Helicobacter pylori).
- analgesic properties.
Additionally, other studies have shown that oral probiotic microbes can reduce anxiety and stress . All of this is related to the already discussed microbiome-gut-brain axis.
A New Horizon of Nutrition
The conclusion to all this is that there is still a lot to study and investigate and above all to reaffirm with replicable models the metabolic routes by which Nutritional Psychiatry works since being something so new there are still some scientific bases to confirm even though they are already mentioned.

If we pay attention, almost all these nutritional treatments ask for a diet mostly based on plants or foods of plant origin, very few foods of animal origin, and no highly processed foods. An inclination towards a vegan or vegetarian lifestyle has to be made to improve health. What all these studies tell us is that we must frequent and promote a balanced diet based on foods of plant origin and try to avoid at all costs the factors that suppress and affect the metabolic pathways that affect our mental health.